Ayushman Bharat Yojana (ABY), also known as Pradhan Mantri Jan Arogya Yojana (PMJAY), is a game-changer in India’s healthcare landscape. Launched by the government, it aims to shield underprivileged families from the burden of medical expenses.
This article covers detailed information about the eligibility criteria, required documents, and more.
Contents
- 1 Overview of Ayushman Bharat Yojana
- 2 What is the Ayushman Bharat Yojana?
- 3 Benefits of the Ayushman Card Scheme
- 4 Eligibility for Ayushman Bharat Yojana Rural
- 5 Eligibility Criteria for Urban Families
- 6 Documents Required for Ayushman Bharat Yojana
- 7 How to apply for Ayushman Bharat Yojana?
- 8 How to check the PM-JAY card application status?
- 9 FAQs
Overview of Ayushman Bharat Yojana
Ayushman Bharat Yojana is a health insurance scheme launched by the Government of India. The scheme aims to provide health insurance coverage to economically vulnerable people in India. The Central Government provides economic strength to poor citizens by running the Ayushman Bharat Scheme.
| Name of Scheme | Ayushman Bharat Yojana |
|---|---|
| Launch Date | September 23, 2018 |
| Coverage (per family) | Rs. 5 Lakh per year |
| Pre-hospitalization Coverage expenses | Upto 3 days |
| Post-hospitalization Coverage expenses | Upto 15 days |
| Official Website | https://www.pmjay.gov.in/ |
| Helpline Number | 1800-111-565 |
| Email ID | [email protected] |
What is the Ayushman Bharat Yojana?
Ayushman Bharat is a health protection scheme that aims to provide health insurance to citizens in India. Under this scheme, beneficiaries receive insurance coverage of up to Rs. 5 lakh annually on a family floater basis. This coverage is intended to help individuals access primary, secondary, and tertiary healthcare services.
Initially known as AB-NHPS under the National Health Protection Scheme (NHPS), it is now called Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (PM-JAY). The government plans to implement this scheme through national insurance companies.
Ayushman Bharat PM-JAY amalgamates the existing senior citizen health insurance scheme and the Rashtriya Swasthya Bima Yojana.
Benefits of the Ayushman Card Scheme
This scheme aims to provide free health insurance facilities up to Rs 5 lakh to citizens from the Economically Weaker section.
Here are the specifics of this scheme –
- Coverage: Covers up to 3 days of pre-hospitalization expenses, 15 days post-hospitalization expenses, all pre-existing conditions, drugs, supplies, diagnostic services, physician’s fees, room charges, surgeon charges, OT and ICU charges
- No restrictions: There is no restriction on age, family size, or gender.
- Portable: Benefits are available PAN India
- Special packages: Provides special packages for women-related health issues, including maternity care, cervical cancer, breast cancer, and other reproductive health concerns
- Covers a wide range of diseases: Cardiovascular diseases, various types of cancer, orthopedics, neurological conditions, kidney disease, respiratory diseases, mental health, overall maternal and child health, diabetes, hypertension, and gastrointestinal disorders
Eligibility for Ayushman Bharat Yojana Rural
These are the criteria to identify the rural families –
- Families that do not have an earning adult member aged between 16 and 59 years.
- Households headed by female members having no adult male members aged between 16 and 59 years.
- Households with a single room have makeshift walls and roofs.
- Households belonging to the Scheduled Castes and Scheduled Tribes categories.
- Households that have disabled members with no able members offering support.
- Landless households with manual labor as their basic source of income.
In addition, the following households are automatically eligible –
- Destitute families who rely on alms.
- Families of manual scavengers.
- Households without proper shelter.
- Families of bonded labor.
- Primitive and particularly vulnerable tribal groups.
Eligibility Criteria for Urban Families
- Street vendors, cobblers, and hawkers.
- Domestic workers.
- Rag pickers and beggars.
- Construction site workers, plumbers, masons, painters, welders, and security guards.
- Coolies.
- Sweepers, sanitation workers, and gardeners.
- Transport workers such as conductors, drivers, cart pullers, and others.
- Artisans, home-based workers, handicraft workers, and tailors.
- Washermen and watchmen.
- Electricians, mechanics, repair workers, and assemblers.
- Peons, helpers, shop workers, delivery assistants, attendants, and waiters.
Documents Required for Ayushman Bharat Yojana
Here are the documents required to register for Ayushman Bharat Yojana –
- Adhaar card
- Residency proof
- Family details
- Income certificate
- Caste certificate
- Bank Details
How to apply for Ayushman Bharat Yojana?
You need to follow these simple steps to apply for this scheme –
Step 1: Visit the official website
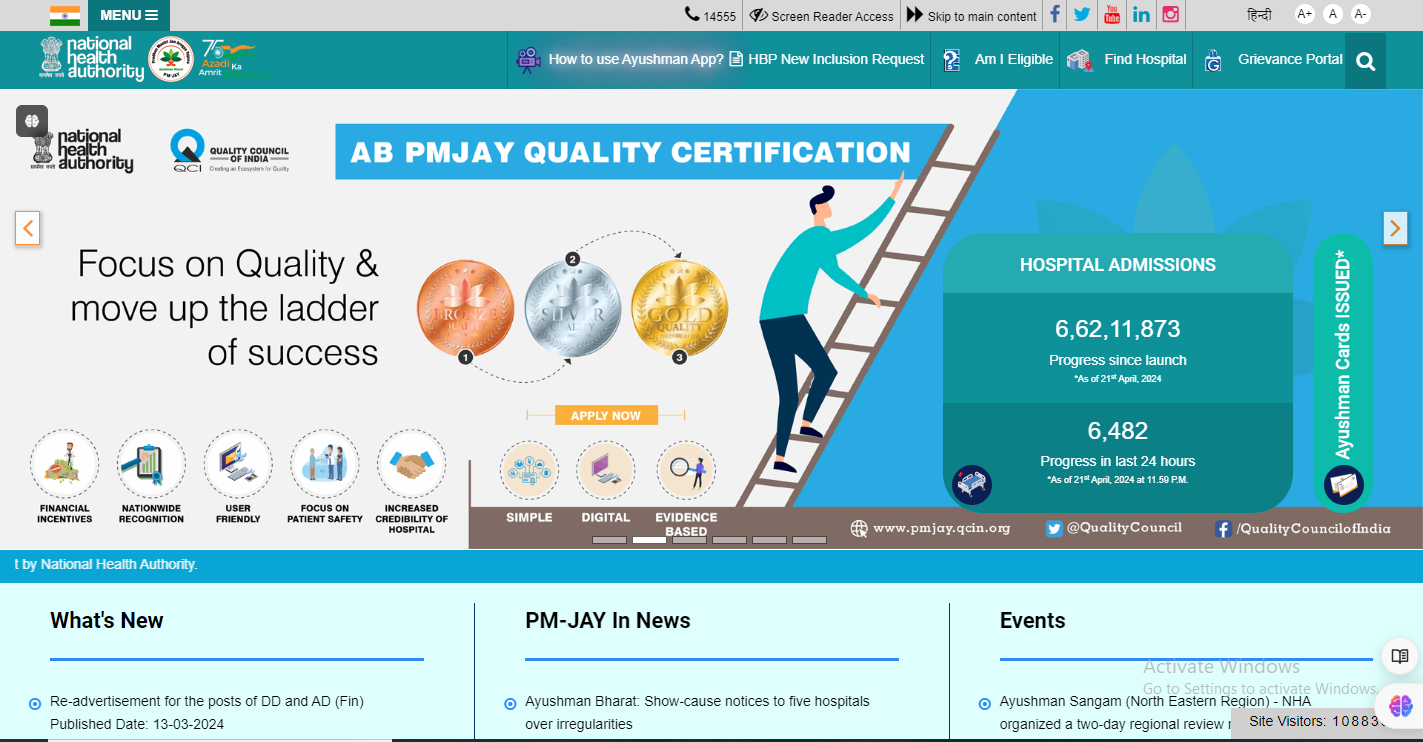
First of all, visit the official website of PMJAY at https://www.pmjay.gov.in/.
Step 2: Apply for PM-JAY
Scroll down to the Apply for PM-JAY section and click on it.
Step 3: Provide your details
Enter the essential details that will include your mobile number, Aadhar card, and other details.
Step 4: Upload documents
Upload the scanned copies of the required documents.
Step 5: Submit the registration form
Recheck all the information and documents provided and submit the Registration form.
After submitting the form, you will receive an acknowledgment message with a reference number. Use this reference number to track the status of your application.
How to check the PM-JAY card application status?
After successfully applying, you will receive an approval message within 9-10 days. In case you haven’t received the message, you can follow these steps to monitor the status of your application through the PM-JAY portal –
- Visit the official PM-JAY website.
- Scroll down to the “Application Status” section on the portal.
- Enter the asked details, including your reference number given at the time of application.
- Application Portal will now provide you with the information regarding the status of your PM-JAY card application.
You may like to read –
- PM Awas Yojana 2024 List, Application, and More
- Bihar Mukhyamantri Laghu Udyog Yojana Released
- Balika Protsahan Yojana: Application Process, Eligibility, and Benefits
FAQs
Can a newborn be covered under PMJAY if five family members have already benefited from it?
Yes, there is no limit to the size of the family under the PMJAY. Newborn babies will receive care under the PMJAY as long as the benefit limit is not reached.
What are the services that are excluded under the PMJAY?
Outpatient care, cosmetic treatments, drug rehabilitation, fertility treatment, and organ transplants are not covered under the PMJAY.
Does a beneficiary need to pay for medicines he/she receives under this scheme?
No, beneficiaries do not need to pay for the medications they receive for treatment. Medications are covered under the PMJAY package for the entire treatment period, including up to 15 days after discharge from the hospital.